ACBH QA FAQs
|
CANS / NOABD / COVID-19 / SMHS / Timeliness Welcome to the Alameda County Behavioral Health (ACBH) Quality Assurance Department Frequently Asked Questions (FAQ’s) page. This page will assist you in answering our most frequently asked questions related to Clinical Documentation Standards, Medi-Cal Site Certification, Audits, and other QA ActivatesThe available FAQs are reviewed quarterly to provide you with pertinent tools for the delivery of services to ACBH consumers.
Select your topic above to search for you question. Can’t find your question? Email our ACBH Quality Assurance clinical team at qata.acgov.org for further assistance. CANS & PSC FAQs
| ||||||||||||||||||||||||||||||||||||||||||||||||
| Provider Type | Type of NOABD likely used |
|---|---|
| SMHS Adult | Termination
Timely-Access Grievance only if your manage your own Grievance System |
| SMHS Children’s/Access Point | Denial
Delivery Modification Termination Timely-Access Grievance only if your manage your own Grievance System |
| SUD Tx | Denial
Termination Timely-Access Grievance only if your manage your own Grievance System |
All NOABDs shall be reported to ACBH QA Office via Fax: 510.639.1346 or Mail to: 2000 Embarcadero Cove, Suite 400, Oakland, CA 94606
Regulations:
Establishing Medical NecessityMental Health Services for Adults: CCR 1830.205
Medical Necessity Criteria for MHP Reimbursement of Specialty Mental Health Services.
(a) The following medical necessity criteria determine Medi-Cal reimbursement for specialty mental health services that are the responsibility of the MHP under this Subchapter, except as specifically provided.
(b) The beneficiary must meet criteria outlined in Subsections (1)-(3) below to be eligible for services:
(1) Have one of the following diagnoses in the Diagnostic and Statistical Manual of Mental Disorders, DSM-IVE, Fourth Edition (1994), published by the American Psychiatric Association:
(A) Pervasive Developmental Disorders, except Autistic Disorders
(B) Disruptive Behavior and Attention Deficit Disorders
(C) Feeding and Eating Disorders of Infancy and Early Childhood
(D) Elimination Disorders
(E) Other Disorders of Infancy, Childhood, or Adolescence
(F) Schizophrenia and other Psychotic Disorders, except Psychotic Disorders due to a General Medical Condition
(G) Mood Disorders, except Mood Disorders due to a General Medical Condition
(H) Anxiety Disorders, except Anxiety Disorders due to a General Medical Condition
(I) Somatoform Disorders
(J) Factitious Disorders
(K) Dissociative Disorders
(L) Paraphilias
(M) Gender Identity Disorder
(N) Eating Disorders
(O) Impulse Control Disorders Not Elsewhere Classified
(P) Adjustment Disorders
(Q) Personality Disorders, excluding Antisocial Personality Disorder
(R) Medication-Induced Movement Disorders related to other included diagnoses.
(2) Have at least one of the following impairments as a result of the mental disorder(s) listed in Subsection (b)(1) above:
(A) A significant impairment in an important area of life functioning.
(B) A reasonable probability of significant deterioration in an important area of life functioning.
(C) Except as provided in Section 1830.210, a reasonable probability a child will not progress developmentally as individually appropriate. For the purpose of this Section, a child is a person under the age of 21 years.
(3) Meet each of the intervention criteria listed below:
(A) The focus of the proposed intervention is to address the condition identified in Subsection (b)(2) above.
(B) The expectation is that the proposed intervention will:
1. Significantly diminish the impairment, or
2. Prevent significant deterioration in an important area of life functioning, or
3. Except as provided in Section 1830.210, allow the child to progress developmentally as individually appropriate.
4. For a child who meets the criteria of Section 1830.210(1), meet the criteria of Section 1830.210(b) and (c).
(C) The condition would not be responsive to physical health care based treatment.
(c) When the requirements of this Section or Section 1830.210 are met, beneficiaries shall receive specialty mental health services for a diagnosis included in Subsection (b)(1) even if a diagnosis that is not included in Subsection (b)
(1) is also present.
Note: Authority cited: Section 14680, Welfare and Institutions Code. Reference: Sections 5777 and 14684, Welfare and Institutions Code.
Mental Health Services for Children: CCR 1830.210
Medical Necessity Criteria for MHP Reimbursement for Specialty Mental Health Services for Eligible Beneficiaries Under 21 Years of Age.
(a) For beneficiaries under 21 years of age who are eligible for EPSDT supplemental specialty mental health services, and who do not meet the medical necessity requirements of Section 1830.205(b)(2)-(3), medical necessity criteria for specialty mental health services covered by this Subchapter shall be met when all of the following exist:
(1) The beneficiary meets the diagnosis criteria in Section 1830.205(b)(1),
(2) The beneficiary has a condition that would not be responsive to physical health care based treatment, and
(3) The requirements of Title 22, Section 51340(e)(3)(A) are met with respect to the mental disorder; or, for targeted case management services, the service to which access is to be gained through case management is medically necessary for the beneficiary under Section 1830.205 or under Title 22, Section 51340(e)(3)(A) with respect to the mental disorder and the requirements of Title 22, Section 51340(f) are met.
(b) The MHP shall not approve a request for an EPSDT supplemental specialty mental health service under this Section or Section 1830.205 if the MHP determines that the service to be provided is accessible and available in an appropriate and timely manner as another specialty mental health service covered by this Subchapter and the MHP provides or arranges and pays for such a specialty mental health service.
(c) The MHP shall not approve a request for specialty mental health services under this Section in home and community based settings if the MHP determines that the total cost incurred by the Medi-Cal program for providing such services to the beneficiary is greater than the total cost to the Medi-Cal program in providing medically equivalent services at the beneficiary's otherwise appropriate institutional level of care, where medically equivalent services at the appropriate level are available in a timely manner, and the MHP provides or arranges and pays for the institutional level of care if the institutional level of care is covered by the MHP under Section 1810.345, or arranges for the institutional level of care, if the institutional level of care is not covered by the MHP under Section 1810.345. For the purpose of this Subsection, the determination of the availability of an appropriate institutional level of care shall be made in accordance with the stipulated settlement in T.L. v. Belshe.
Note: Authority cited: Section 14680, Welfare and Institutions Code. Reference: Sections 5777, 14132 and 14684, Welfare and Institutions Code; Title 42, Section 1396d(r), United States Code; and T.L. v. Belshe, United States District Court, Eastern District of California, Case No. CV-S-93-1782 LKK PAN.
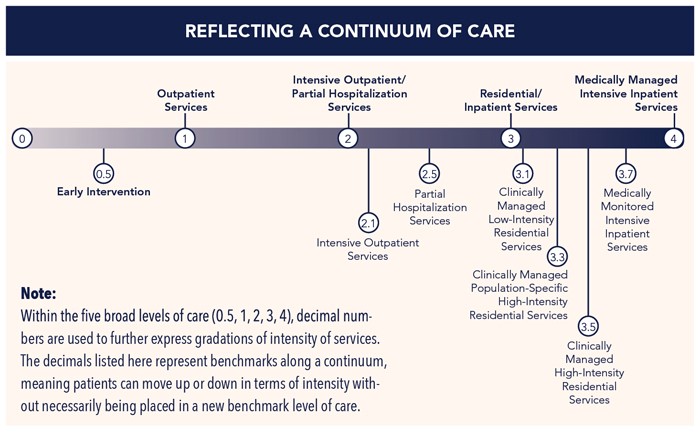
Substance Use Disorder: ASAM Levels of Care
ASAM Levels of Care Criteria
The ASAM Criteria text describes treatment as a continuum marked by four broad levels of service and an early intervention level. Within the five broad levels of care, decimal numbers are used to further express gradations of intensity of services. These levels of care provide a standard nomenclature for describing the continuum of recovery-oriented addiction services. With the ASAM CONTINUUM™, clinicians are able to conduct a multidimensional assessment that explores individual risks and needs, as well as strengths, skills and resources. ASAM CONTINUUM then provides clinicians with a recommended ASAM Level of Care that matches intensity of treatment services to identified patient needs.
| Do you have a question?
Need Technical Assistance? |
Contact QA Technical Assistance |
|---|
SPECIALTY MENTAL HEALTH SERVICES (SMHS) FAQ’S 
Index:
- Assessment: Cultural & Linguistic Considerations; Diagnoses; Safety;
- ACBHCS System of Care Auditing
- Beneficiary Rights
- CANS/ANSA Documentation Standards
- Claiming SMHS
- Grievances & Appeals
- Informing Materials
- Medicare-Medi-Cal Concurrent Claiming
- Scope of Practice
- Therapeutic Behavioral Services
- Day Rehabilitation & Day Treatment Intensive
- Client Plans
What Sexual Orientation and Gender Identity/Expression (SO/GIE) data must be collected at Initial and Annual Assessment.
A. The fields are as follows:
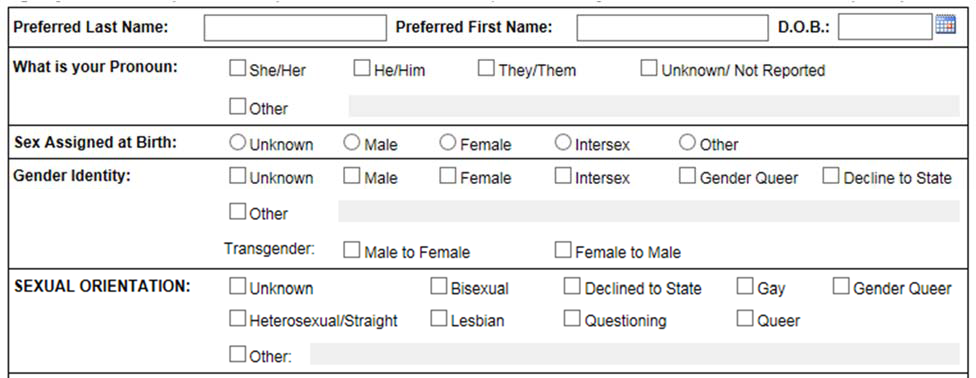
For Pronoun, Gender Identity & Sexual Orientation—select all that apply.
Are there other SO/GIE considerations when developing the Assessment template or when inquiring with the client and/or family? A1. Yes, rather than asking about Mother or Father, ask about Parents, Caretakers (inclusive of extended family) or Guardians.
A2. Also, rather than asking is someone is married or has a husband or wife, ask if they have a Significant Other or Domestic Partner.
Assessment- Diagnoses
What are the charting diagnoses requirements?
A. Diagnoses documented in the client’s clinical record, such as a paper chart or an EHR, must represent the client’s full DSM-5 diagnostic picture. It must include the same diagnoses entered into InSyst, plus any additional diagnoses the client may have. Diagnoses in the clinical record must be supported by documentation including: specific signs, symptoms, and timeframes of the diagnoses that client exhibits—unless it is a diagnosis gathered “by history” and is not a focus of treatment. All Diagnoses must include the ICD-10 code and the appropriate DSM descriptor (diagnosis name) with specifiers and severity (when appropriate).
Assessment - Safety
If a client is found to have suicidal/homicidal/other significant risk ideation is a Safety Plan required?
A. Yes, if at any point ideation is identified (having occurred anytime in the past 90 days) --both a comprehensive Risk Assessment AND a formal written Safety Plan must be developed in coordination with the client. Also, see Q2 below.
What if a client has a history of suicidal/homicidal/other significant risk ideation but is currently stable and has these symptoms controlled.
A. ACBHCS requires that if a client has had any a suicidal/homicidal/other significant risk ideation in the past 90 days that both a comprehensive Risk Assessment AND a formal written Safety Plan must be developed in coordination with the client. If it has been more than 90 days since the client last experienced symptoms of suicidal/homicidal/other significant risk ideation the clinical situation must be considered carefully to determine if a comprehensive Risk Assessment AND a formal Safety Plan should be completed. Beyond 90 days of ideation, if it is determined that a Comprehensive Risk Assessment and formal written Safety Plan are not indicated, document the clinical reasoning for this decision.
What elements must be documented in a comprehensive Risk Assessment and formal Safety Plan?
A. The Comprehensive Risk Assessment must be documented in the Clinical Record. The Safety Plan must also be documented in writing and provided to the client as a resource for reference as needed. It is crucial that the development of the Plan is a clinical process and that each step is embraced and endorsed by the client.
ACBHCS System of Care Auditing:
When a chart is chosen by Alameda County to be audited, will the county recoup money for progress notes/claims that fail to meet Medi-cal ACBHCS documentation standards?
A. All providers and regulators have a legal and ethical duty to reduce fraud, waste, and abuse. All claims during the audit period (often 3 months of services) are examined to assure that the services provided support the claims associated with them. If documentation does not meet minimum documentation requirements to support the service/claim, Alameda County will recoup those funds and return them to the funding source.
What is a quality comment? Will a claim be recouped if there is a quality comment about it?
A. Often charts will include enough information to support the claim but will have quality issues. In these instances, feedback describing the quality issues will be provided and require a Quality Improvement Plan on the part of the agency to assure improved documentation in the future. These claims are not recouped, but such future claims with poor quality may be recouped--especially if a program fails to improve the quality of their documentation in the future.
Why are claims outside of the audit period recouped?
A. In the course of reviewing a chart, if it is determined that claims outside of the audit period are also not supported by documentation in the chart, there is a legal and ethical duty to recoup those funds and return them to the funding source.
What type of documentation problems would cause claims outside of the audit period to be identified as needing recoupment?
A. The most common reasons for claims outside the audit period being recouped include:
1: Assessments reviewed were: not completed, not signed, late, etc. (see DHCS Reasons for Disallowances with ACBHCS Comments).
2: Treatment plans reviewed were: not completed, not signed, late, or service modality claimed was not listed, etc.
3: The Severity Screening Tool did not support that the client has moderate to severe impairment to functioning and therefore was not eligible for specialty mental health Medi-Cal services. ACBHCS makes available on the county’s web pages the full set of criteria and regulations that are used during the audit process. Please refer to those exhibits for a full list of items that when found deficient will cause claims to be disallowed. http://bhcsproviders.acgov.org/providers/QA/audit.htm
Beneficiary Rights
The MHP Contract (with CA DHCS), Exhibit A, Attachment 3, Item No. 4 states that a beneficiary may "request and receive a copy of his or her medical records, and request that they be amended or corrected." Can providers override such a request if it is not in the best interest of the patient, clinically?
A. This particular beneficiary right incorporates parts of the HIPAA privacy rule. The exact language of Title 42, CFR, Section 438.100(b)(2)(vi) states:
"If the privacy rule, as set forth in 45 CFR parts 160 and 164 subparts A and E, applies, [the beneficiary has the right to] request and receive a copy of his or her medical records, and request that they be amended or corrected, as specified in CFR Secs. 164.524 and 164.526."
Since MHPs are subject to the HIPAA privacy rules, they must grant beneficiaries this right, unless one of the exceptions applies. This is not a brand new requirement; MHPs were already subject to this when the HIPAA privacy rule became effective in April 2003. Title 45, CFR Section 164.524 describes an individual's rights and exceptions to accessing their records. This section (164.524(a)(3)(i)) addresses situations in which accessing the information would not be in the best interest of the beneficiary.
“(i) A licensed health care professional has determined, in the exercise of professional judgment, that the access requested is reasonably likely to endanger the life or physical safety of the individual or another person; (ii) The protected health information refers to another person (unless such other person is a health care provider) and a licensed health care professional has determined, in the exercise of professional judgment, that the access requested is reasonably likely to cause substantial harm to such other person; or (iii) The request for access is made by the individual’s personal representative and a licensed health care professional has determined, in the exercise of professional judgment, that the provision of access to such personal representative is reasonably likely to cause substantial harm to the individual or another person.”
The full text of Title 45, CFR, Section 164.524 can be accessed here: http://edocket.access.gpo.gov/cfr_2009/octqtr/pdf/45cfr164.524.pdf
Title 45, CFR, Section 164.526 describes the amendment process for changing medical records, and the exceptions. The full text of Title 45, CFR, Section 164.526 can be accessed here: http://edocket.access.gpo.gov/cfr_2009/octqtr/pdf/45cfr164.526.pdf.
CANS/ANSA Documentation Standards
When do I need to complete the CANS or ANSA?
A. The CANS or ANSA must be completed at the following timeframes:
- At Opening. The Initial CANS/ANSA must be completed within 60 calendar days of the Episode Opening Date (EOD), but after completion of the MH Assessment and prior to the completion of the Client Plan. CANS/ANSA data/information shall be used to inform the Initial Client Plan.
- At the 6-month mark. A Re-Assessment CANS/ANSA must be completed within the calendar month prior to the 6th month of the EOD.
- At Annual Re-Authorization. A Re-Assessment CANS/ANSA must be completed during the annual re-authorization timeframe which is within the calendar month prior to the episode opening month. CANS/ANSA data/information shall be used to inform the annual Client Plan.
- Upon a clinically significant change. Once the Initial CANS/ANSA is completed, staff must re-administer the CANS/ANSA whenever a clinically significant change occurs or need arises. This CANS/ANSA re-assessment could signal the need to update the Client Plan.
- Client Plan Update (New Plan is created). Conversely, since the CANS/ANSA is used to inform the Client Plan, the CANS/ANSA must be updated with every Client Plan update. That is, when planning to complete a new Client Plan, first administer the CANS/ANSA and then utilize that additional information to inform the new Client Plan.
- At Discharge. A CANS/ANSA must be completed prior to closing the case.
If we complete the CANS or ANSA in the Objective Arts database (rather than on paper form) do I need to print it out?
A. Yes. Since the CANS/ANSA document is part of the official medical record, the print out should be included in the consumer’s chart (medical record). Staff must sign (electronic signature is okay) with credentials, required co-signatures, and date. Completing it by paper for the medical record, or within an Electronic Health Record is also acceptable. However, once the CANS/ANSA is completed on paper—someone will need to do data entry of the results into the Objective Arts database which is not a claimable service.
I’m credentialed as a MHRS or Adjunct Staff; can I complete the CANS or ANSA?
A. No. Due to the clinical nature of the CANS/ANSA, staff who completes a CANS/ANSA must meet the credentialing standards as in the category of Evaluation (CANS/ANSA) on the BHCS Guidelines for Scope of Practice Credentialing grid. That is, Licensed, or Unlicensed (Waivered or Registered) LPHA’s; OR Graduate MH Student/Trainees). http://bhcsproviders.acgov.org/providers/QA/docs/training/ACBHCS_Guidelines_Scope_ Practice_Credentialing_Provide_Specialty_MH_Services.pdf
How much time may be claimed for scoring and write-up of the CANS/ANSA?
A. The initial CANS/ANSA timeframe is expected to be between 30 – 45 minutes. Updates to the initial CANS/ANS are expected to take between 15 – 20 minutes. (One may use the option to copy the original and then modify for the revised in the CANS/ANSA in the Objective Arts Database.)
Claiming SMHS
What are the Specialty Mental Health Services that are eligible for Medi-Cal reimbursement?
A. Specialty Mental Health Services include: Rehabilitative Mental Health Services, which include:
- mental health services
- medication support services
- day treatment intensive
- day rehabilitation
- crisis intervention
- crisis stabilization
- adult residential treatment services
- crisis residential services
- psychiatric health facility services
- case management—brokerage
- psychiatric inpatient hospital services
- psychiatrist services
- psychologist services
- EPSDT Supplemental Specialty Mental Health Services
Does staff claim travel and documentation time at whatever service function rate, e.g., Mental Health Service (MHS), Case Management, etc., of the service provided?
A. Yes. Travel and documentation time must be linked to the service provided.
Can staff claim Medi-Cal for case management services provided while a beneficiary is in an IMD?
A. FFP cannot be claimed if the beneficiary is between the ages of 22-64. Yes, if the beneficiary is 65 or older. Yes, if the beneficiary is under 21 and is a patient in a hospital or another accredited facility. Follow the specific restrictions indicated for each specific institution (or MH service) as indicated on the ACBHCS Medi-Cal (M/C) Lock-out Grid. http://bhcsproviders.acgov.org/href_files/LockoutSituationsGrid_061517.pdf
Can staff claim Medi-Cal for transporting beneficiaries to mental health appointments as a specialty mental health service?
A. No. Transportation is not reimbursable as a specialty mental health service.
Can staff claim Medi-Cal for a parenting group that includes parents whose children have open cases at the clinic?
A. Yes, if the services are directed at the mental health needs of the children, rather than based upon the needs of the parents. In addition, there must be documentation in the child’s chart to show the need for this activity.
How should time be divided when clients and their parents are seen together in a group setting? Should the time be claimed as mental health services or collateral?
A. Time should be divided equally among the clients being represented. The time should be treated as if this were a group setting composed only of the clients being represented (the parents themselves would not count as group members). Only the time for clients who are Medi-Cal-eligible may be claimed as a Medi-Cal service. For example, a staff meets with three Medi-Cal-eligible clients, five parents of these three clients, and two parents of one Medi-Cal-eligible client who was not present for a total of ten people in a group setting for 120 minutes. Since four beneficiaries were represented, the time is divided by four, and 30 minutes is claimed for each client. If there were an additional client who was not Medi-Cal eligible and that client's parents, the time would be divided by five, and 24 minutes would be claimed for each Medi-Cal eligible client.
When a treatment group contains both Medi-Cal and non Medi-Cal clients, how is staff to divide the time? For example, if a group of six clients containing three Medi-Cal and three non-Medi-Cal clients lasts 120 minutes (group time plus documentation), how is the time divided? By three, or by six?
A. If a provider is delivering services to a group composed of both Medi-Cal and non-Medi-Cal eligible individuals, and the rate is the same, the provider would prorate his or her time for all (6 in above example) individuals who participated.
Can Medi-Cal be claimed for assisting beneficiaries to obtain their medication by preparing an authorization request?
A. Yes, Medi-Cal can be claimed for completing an authorization request for a prescription as it relates to the provision of medication support services. Only physicians, Nurse Practitioners, Physician Assistants, RNs, LVNs, psychiatric technicians, or pharmacists within their scopes of practice may provide medication support services.
Can staff claim Medi-Cal for photocopying, faxing, and other clerical type activities as specialty mental health services?
A. No.
Can staff claim Medi-Cal for payee related activities?
A. Medi-Cal cannot be claimed for time spent performing the fiscal responsibilities of a payee. For example, staff cannot claim Medi-Cal for time spent writing checks to pay the beneficiary’s bills. However, it is possible to claim for payee related services when such activities are necessary to address impairment in an important area of life functioning. For example, staff can claim Medi-Cal for time spent providing training on money management skills.
Can staff claim Medi-Cal for telephone assessments?
A. Yes. Assessments can be completed face-to-face or over the telephone. However, providers are strongly encouraged to complete face-to-face assessments when determining medical necessity.
How long can staff claim Medi-Cal for services provided after a beneficiary has died?
A. All services claimed to Medi-Cal on behalf of a beneficiary must be provided to meet the mental health needs of that beneficiary. Therefore, Medi-Cal cannot be claimed for any services provided once the beneficiary has died. In addition, claims must be submitted in a timely fashion as specified in Title 9.
Can staff claim Medi-Cal for court related assessments, e.g., conservatorship investigations?
A. No, if the assessment is completed per request of the court for a purpose other than determining medical necessity for Medi-Cal. For example, Medi-Cal cannot be claimed if a court-ordered assessment is narrowly defined for establishment of conservatorship and the MHP limits its assessment to this purpose.
What are the current 24-hour claiming limitations listed by service type?
A. California Code of Regulations (CCR), Title 9, Chapter 11, Section 1840.366(b) specifies: "The maximum amount claimable for Crisis Psychotherapy (aka Crisis Intervention) in a 24-hour period is 8 hours." CCR, Title 9, Chapter 11, Section 1840.368(c) specifies: "The maximum number of hours claimable for Crisis Stabilization in a 24-hour period is 20 hours." CCR, Title 9, Chapter 11, Section 1840.372 specifies: "The maximum amount claimable for Medication Support Services in a 24-hour period is 4 hours."
Regarding medication support services, can staff claim Medi-Cal for medication support services in a group setting as long as the following conditions are met: Time is prorated per CCR, Title 9, Chapter 11, Section 1840.316(a)(2), and the medication support services provided meets the definition of medication support services in CCR, Title 9, Chapter 11, Section 1810.225, and The service is provided by staff who are qualified to provide such services?
A. Yes, as in the following example:
An R.N. facilitates a weekly group discussion on medication education, e.g., the side effects of the medication, overcoming resistance to taking medications, etc.
This intervention and its goals should be addressed in each individual's client plan.
Are there any special lockouts on claiming Medi-Cal while a beneficiary is in Rate Classification Level (RCL) 12-14 facilities (group homes that specialize in serving children with mental illness)?
A. There are no special lockouts outside those listed in Title 9 (except for ICC/IHBS services) while a beneficiary resides in RCL 12-14 facilities because the RCL 12-14 rates do not include treatment services. The duplicate payment issues that exist when a beneficiary is in a 24-hour facility that is receiving reimbursement for treatment services do not exist when the beneficiary is in an RCL 12-14 facility.
Can Medi-Cal be claimed for travel time from one provider site to another provider site? How about from a staff person’s residence to a provider site, or from a staff’s home to a client’s home?
A. To claim Medi-Cal, travel time must be from a provider site to an off-site location(s) where Medi-Cal specialty mental health services are delivered. Therefore, Medi-Cal cannot be claimed for travel between provider sites or from a staff member’s residence to a provider site.
NOTE: A "provider site" is defined as a site with a provider number, including affiliated satellite and school site operations.
How long and what types of services can be claimed to Medi-Cal prior to a determination of medical necessity?
A. In an urgent, crisis, or emergency situation, the MHP can/should provide whatever services are needed prior to establishing that all medical necessity criteria are met. If not an urgent, crisis, or emergency situation, the MHP should only claim those assessment services necessary to establish medical necessity.
Alameda has established a maximum 30-day intake period (from the Episode Opening Date – EOD) during which time the provider is to establish medical necessity and complete the MH Assessment with Diagnosis (unless other specified timeframe in the ACBHCS Clinical Documentation Manual). Up to 60 days (from EOD) is allowed to set up the client plan, and coordinate the arrangement of necessary services (unless other specified timeframe in the ACBHCS Clinical Documentation Manual). However, the intake period is not exempt from the medical necessity requirements for claiming Medi-Cal (for example once it is determined that there is not an Included Diagnosis—or any other aspect of Medi- Cal medical necessity is not met—there may be no further claiming, even for MH Assessment or Plan Development).
How does staff claim time when services with two different rates are provided during the course of a client session, e.g., 30 minutes of mental health services and 30 minutes of case management? Does the staff claim the whole time to the dominant service provided, or claims 30 minutes to mental health services and 30 minutes to case management? Can staff write one progress note and break out the claim by each service, or must a separate progress note be written for each service?
A. In the above situation, staff should claim for each service separately or claim the entire time to the lower cost center, e.g., case management. Staff may write two separate progress notes or write one progress note that clearly delineates the time spent providing each service.
- Example One: One note for 60” Case Management written and claimed with delineation in body of PN that 30” was spent on MH Services (such as Individual Therapy) and 30” was spent of Case Management.
- Example Two: Two notes written and claimed. One for 30” Case Management and one note for 30” MH Service (such as Ind Therapy).
When can Medi-Cal be claimed for treating undocumented individuals?
A. The MHP needs to deliver services to beneficiaries who are undocumented individuals based on what is covered by the beneficiaries’ aid category. Undocumented individuals are eligible for aid categories that cover emergency and/or pregnancy services only.
Title 9, California Code of Regulations (CCR), Section 1810.216 says: "'Emergency Psychiatric Condition' means a condition that meets the criteria in Section 1820.205 when the beneficiary with the condition, due to a mental disorder, is a danger to self or others, or immediately unable to provide for or utilize, food, shelter or clothing, and requires psychiatric inpatient hospital or psychiatric health facility services."
What this means is that only emergency psychiatric inpatient hospital services and related psychiatric inpatient hospital professional services are covered for Medi-Cal beneficiaries who are only covered for emergency services. Crisis intervention and crisis stabilization are not emergency services under the Medi-Cal managed mental health care program. Pregnancy-related services, when covered, are broader than emergency services. These services involve treatment of a mental illness that might affect the outcome of the pregnancy. A Provider’s contract may include the provision of non-Medi-Cal services to undocumented individuals, or others without Medi-Cal.
If a patient is admitted to an acute care setting for a medical condition, what specialty mental health services are eligible for Medi-Cal?
A. CCR, Title 9, Section 1840.215 and Sections 1840.360 through 1840.374 only address lock-out requirements for specialty mental health services. There is nothing in the regulations that prohibits claiming Medi-Cal for the provision of medically necessary specialty mental health services while a beneficiary is on a medical unit. See ACBHCS Medi-Cal Lock-out Grid.
Can Medi-Cal be claimed for administrative hospital days if Medi-Cal was not claimed for the days of acute status? For example, a patient who otherwise meets medical necessity criteria but is ineligible for Medi-Cal because of his/her legal status, e.g., in jail custody. The court later releases him/her, but the patient remains in the hospital pending suitable placement.
A. Yes, as long as medical necessity for acute psychiatric inpatient hospital services had been established at some point during the patient’s stay in the hospital and the administrative days meet criteria specified in CCR, Title 9, Section 1820.220(j)(5).
What are the rules around claiming Medi-Cal for services provided by students, volunteers, and paid consumers?
A. Generally: 1) A "student" (aka trainee) is someone who is in school in a social work, counseling, or related school placement program at a provider site and includes both undergraduate and graduate students. 2) A “volunteer” is someone who is not "employed" by the provider, for example, a person accumulating qualifying hours to become licensed, and works without pay. 3) A “paid consumer” is someone who is a consumer and who is employed by the provider, typically to provide peer support and interaction to the provider’s clients. As long as all Medi-Cal requirements and any supervision and scope of practice requirements are met, providers may claim for Medi-Cal services provided by students, volunteers, and paid consumers (all additional provider credentialing requirements remain the same.) See ACBHCS Medi-Cal Lock-out Grid.
What are the requirements of diagnoses entered into InSyst and how does this differ from documenting the diagnoses in the client’s clinical record?
A. InSyst is part of the county and state’s Medi-Cal billing system, diagnoses entered into InSyst should relate to claims made to Medi-Cal. Only select mental health diagnoses approved by DHCS may be treated under Medi-Cal services and are also known as Included Diagnoses. Only treatment for Included diagnoses may be claimed to Medi-Cal and as such only those diagnoses are required to be inputted in to InSyst. Additional (non-treated) diagnoses may be entered into InSyst, but some may not be allowed. SMHS Inpatient, SMHS Outpatient, and SUD services have different Included Diagnoses lists that can be found on the BHCS Provider website. Providers must use the appropriate Included list for their type of services. Please see the Quality Assurance section of the ACBHCS Provider Website for the M/C Included Diagnoses Lists.
Grievances and Appeals
What is the definition of "grievance"? If there are no more "informal complaints," what qualifies as an issue that must follow the resolution process, and what does not? When does a verbal 'bad hair day' remark transition into a verbal grievance? How do we decide if little gripes have to follow a formal grievance process?
A1. Per Title 42, CFR, Section 438.400(b), “grievance” means an expression of dissatisfaction about any matter other than an “action.” If a beneficiary decides to use the MHP process to file a grievance, i.e., telling the designated grievance staff person, filling out a form, etc. for a minor issue then the provider needs to follow the grievance process. If the beneficiary makes a remark to a receptionist, clinician, etc., in passing, but does not want to pursue further action, then they are not required to do so. Or, if a beneficiary makes a comment directly to their clinician, or another MHP staff person, but just wants to "vent," that beneficiary does not have to file a grievance with the MHP. In this example, the clinician, or other MHP staff person, should take the opportunity to remind the beneficiary of the available problem resolution processes.
Informing Materials
Must providers utilize the ACBHCS developed Informing Materials?
A. Yes, however, providers may add additional documents to the Informing Materials packet.
What Scope of Practice must staff hold in order to explain (and answer questions regarding) the ACBHCS required Informing Materials Packet?
A1a. Any staff may explain and answer questions with the proper training, knowledge and experience for the following items in the Packet: Freedom of Choice; Explanation of the Provider Referral List, the Guide to Medi-Cal Mental Health Services & the BHP Member Handbook; Advance Directive Information; Beneficiary Problem Resolution Information; and Maintaining a Welcoming & Safe Place (not a required informing material). The Progress Note must document this discussion and be signed by the provider.
A1b. Only staff whose Scope of Practice includes conducting MH Assessments may explain and answer questions regarding: Consent for Services; Confidentiality & Privacy statement (Duty to Report); and the Notice of Privacy Practices (HIPAA/HITECH). This is limited to Graduate MH Students/Trainees and (Board Licensed, Waivered or Registered) LPHA’s. As this discussion may elicit sensitive clinical concerns (such as abuse or neglect), it must be held in a private confidential setting. The Progress Note must document this discussion and be signed by staff with these credentials.
Medicare-Medi-Cal Concurrent Billing
What constitutes a service provided by telephone and how is billing coded?
A1. Services provided by telephone differ from telemedicine services. Tele-medicine benefits are Medicare reimbursable when provided from a clinic through interactive voice and visual interface between the provider and the client and when provided in specific, eligible geographic regions. Services provided via telemedicine should be claimed to Medicare prior to Medi-Cal unless another exception to prior Medicare claiming exists. Specialty mental health services provided over the telephone are not Medicare reimbursable and should be billed directly to Medi-Cal. When a service is delivered by telephone, the appropriate place of service code should be indicated as “telephone”.
How is place of service "03" (School) defined?
A. A facility whose primary purpose is education.
How is place of service "15" (Mobile Unit) defined?
A. A facility/unit that moves from place-to-place and equipped to provide preventive, screening, diagnostic, and/or treatment services.
How should the service activity "Plan Development” under "Mental Health Services" be billed for Medi-Medi claims?
A4. Plan Development is a service activity under Mental Health Services that is not Medicare reimbursable regardless of where it is provided, or who provides it. When claiming the service activity Plan Development under Mental Health Services bill Medi-Cal directly for Medi-Medi clients.
How should the service activities “Assessment”, “Therapy”, and “Collateral” under "Mental Health Services" be billed for Medi-Medi claims?
A. These must be claimed to Medicare prior to Medi-Cal, unless an exception to Medicare billing exists (for example, the service is provided over the telephone or in the community, it is provided by a non-Medicare reimbursable provider, or in a non-Medicare reimbursable place of service).
Scope of Practice
Regarding the AA degree referenced in Title 9, CCR, Section 630, defining a Mental Health Rehabilitation Specialist, can two years of college be substituted for the AA degree?
A. Receipt of an AA degree is an absolute. Two years of college cannot substitute for it. Title 9, CCR, Section 630, reads: "A mental health rehabilitation specialist shall be an individual who has a baccalaureate degree and four years of experience in a mental health setting as a specialist in the fields of physical restoration, social adjustment, or vocational adjustment. Up to two years of graduate professional education may be substituted for the experience requirement on a year-for-year basis; up to two years of post-associate arts clinical experience may be substituted for the required educational experience in addition to the requirement of four years' experience in a mental health setting." See Table #1 below.
| TABLE 1: MHRS REQUIREMENTS | |
|---|---|
| Educational Degree (any subject) | Experience (specialist in field of physical restoration, social adjustment or vocational adjustment in a MH Setting) |
| AA/AS | 6 years |
| BA/BS | 4 years |
| MS/MA or PhD/PsyD and not Licensed/Waivered/Registered | 2 years |
Therapeutic Behavioral Services
What are the qualifications for a TBS provider?
A. TBS may be provided by a Licensed Practitioner of the Healing Arts (LPHA), or staff that is under the direction of a LPHA to provide TBS. The TBS Clinician is an LPHA and is responsible for the treatment plan establishing goals and is the Medi-Cal provider. The TBS Coach is under the direct supervision of the TBS Clinician and implements the TBS Treatment plan with the approval/supervision of the TBS Clinician.
Where can the training information and manuals mentioned in DMH Information Notice 08-38 be found? Who do we contact to receive these materials and the technical assistance needed to implement the new requirements?
A. DMH/DHCS worked with the California Institute for Mental Health (CiMH) to develop the training materials mentioned in DMH Information Notice 08-38. The TBS Documentation Manual and the TBS Best Practices Manual are available on the website below. In addition, subscribe to TBS information on the DMH website for up to date details on the training materials as well as all other TBS information. http://www.dhcs.ca.gov/services/mh/Pages/EPSDT.aspx
Who can provide Specialty Mental Health Services to children receiving TBS?
A. A provider is defined in the California Code of Regulations (CCR), Title 9, and Section 1810.235 as any person or entity who is licensed, certified, or otherwise recognized or authorized under state law governing the healing arts to provide specialty mental health services and who meets the standards for participation in the Medi-Cal program. Providers include, but are not limited to, licensed mental health professionals, clinics, hospital outpatient departments, certified day treatment facilities, certified residential treatment facilities, skilled nursing facilities, psychiatric health facilities, general acute care hospitals, and acute psychiatric hospitals that are under contract with the MHP.
Can TBS be a “stand alone” mental health service or does the client need to have an open mental health case with the MHP?
A. TBS can never be a “stand alone” mental health service. TBS is considered short term and supplemental to other Specialty Mental Health Services. Specialty Mental Health Services are defined in CCR, Title 9, Section 1810.247 as rehabilitative mental health services, psychiatric inpatient hospital services, targeted case management, psychiatrist services, psychologist services, EPSDT supplemental specialty mental health services, and psychiatric nursing facility services. http://www.dhcs.ca.gov/services/mh/Pages/EPSDT.aspx
Are there TBS Manuals?
A. Yes: Therapeutic Behavioral Services Coordination of Care Best Practices Manual 2.0 - 12/21/2010 & Therapeutic Behavioral Services (TBS) Documentation Manual 2.0: To support the implementation of the Court’s approved Nine Point Plan, the Department developed the TBS Documentation Manual to guide counties and other key stakeholders on how to document and claim TBS appropriately.
Day Treatment
[Day Rehabilitation (DR) or Day Treatment Intensive (DTI)]
Assessment window: if a child is admitted to day treatment without a recent assessment, is an assessment “window” available to establish the service necessity, as in Coordinated Care?
A. Providers are required to seek initial authorization for day treatment services and prior authorization for day treatment services that exceed five days per week.
Staff available to the milieu: is this requirement met if staff is in the milieu room but working individually with a child? On site (in another room) but working with one child or awaiting a need for their intervention?
A. Day treatment staff must be available where and when day treatment therapeutic milieu is being provided and available to respond to the needs of the group. At least one staff person must be available to the group in the therapeutic milieu. Staff in the milieu room working with an individual beneficiary would be considered staff available to the milieu. Staffing ratios must be maintained. Staff on site, but in another room working with one client or waiting for the need for intervention would not be considered staff available to the milieu. If a beneficiary requires such a high degree of one-to-one interaction that staffing ratios are jeopardized or that other day treatment beneficiaries do not have access to the staff, the day treatment program may not be appropriate to meet the needs of the beneficiary and other interventions should be considered. The provision of day treatment is an interactive process. Day treatment staff should not be simply awaiting a need to intervene. Staff should be actively involved the entire time the day treatment program is in operation providing therapeutic interventions to the group. It is reasonable to anticipate that one beneficiary might require additional attention at some time; however, the day treatment staff should use the milieu environment to support the intervention. For example: One beneficiary habitually interferes with other beneficiaries in a group process. The day treatment staff would use the input of the other group members to identify the behavior, to identify why the behavior is problematic and to develop interventions.
Continuous hours of operation: if staff is fully integrated into a classroom during academic instruction, may the school day hours be counted as part of the continuous hours? If so, must staff be present in the classroom to be counted as fully integrated?
A. The hours of the day treatment milieu must be continuous and are not tied to the hours of the setting in which they are provided (e.g., school). The day treatment milieu may operate for a continuous period of time during the school day, but may not be provided in discontinuous "blocks" of time, e.g., two hours in the morning, two hours in the afternoon and one hour after school. The day treatment milieu establishes the hours of operation and must exceed four hours per day for full day programs and be at least three hours per day for half-day programs. In addition to required hours of operation, full-day programs require an average of three treatment hours and half-day program require an average of two treatment hours per day in the day treatment milieu. The community meeting time is not counted in the required treatment hours, but may be a part of the continuous hours of operation/therapeutic milieu or may be separate. (If the community meeting time is not continuous with the therapeutic milieu; the meeting time would not count toward the required hours of operation for a full-day or half day program.) If day treatment is taking place in a school setting, day treatment staff must be present during day treatment time. In cases where staff members work for both a day treatment program and another program (e.g., school), there must be a clear audit trail which documents that staff time and activities are exclusively allocated to one program at a time. The staff must only be counted in one staffing ratio at a time, i.e., while the staff is working in the day treatment program, the staff may not be counted in the school program staffing ratio and vice-versa. See Table 2 below.
Length of stay: is there any sort of expectation about how long a client could/should remain in day treatment?
A. Clinical decisions and determinations to continue or discontinue day treatment or any other specialty mental health service must be based on the individual treatment needs of the beneficiary. Providers are responsible for monitoring beneficiaries' progress in day treatment to determine when client plan goals have been met and to determine when day treatment should be continued, reduced, or terminated.
| TABLE 2: DAY TREATMENT (DR & DTI) HOURS | ||
|---|---|---|
| Type of Hours | Half Day Program | Full Day Program | Minimum hours of Operation (continuous therapeutic milieu) | 3 hours | > than 4 hours | Minimum average daily hours of service components (psychotherapy, process groups, skill building groups, and adjunctive therapies groups) must be made available | 2 hours | 3 hours |
Minimum attendance: must a child be in the milieu for over 50% of the day for billing to be allowed? Or, could some of the time be spent in individual services apart from the milieu but not separately billed, or in transitioning to a mainstream classroom?
A. Beneficiaries are expected to be present in the day treatment program for all scheduled hours of operation of the day treatment program. When a beneficiary is unavoidably absent for some part of the hours of operation, day treatment for an individual beneficiary will only be reimbursed if the beneficiary is present for at least 50% of the hours of the scheduled hours of that day. Individual services may be part of the day treatment program, provided the minimum day treatment requirements are met for the beneficiary. There are no exceptions to these requirements for children being transitioned to a mainstream classroom.
Authorization: must a number of service units be requested for authorization, or only the type of service?
A. Day treatment authorizations must address the total number of days for which the service is authorized. The number of days per week as well as the length of calendar time must be specified. Authorizations which exceed five days a week must be prior authorized by ACBHCS. Mental health services as defined in Title 9, California Code of Regulations (CCR), Section 1810.227, excluding services to treat emergency and urgent conditions and therapeutic behavioral services, provided to a beneficiary on the same day as day treatment must be prior authorized by the MHP. ACBHCS must establish that the additional services are medically necessary considering that the beneficiary is also receiving day treatment. The authorization period for the mental health services (as defined above) must identify when reauthorization, if necessary, will be required and cannot exceed the timeframes for authorization of the day treatment program. Generally, authorization of the type of service and the number of units within the authorization period would be the most effective way to achieve these goals. ACBHCS may use alternate methods, as long as these goals are met.
Activities outside program hours: how can the required contact with caregivers, travel, documentation, etc. be distinguished from non-day treatment activities such as collateral contacts?
A. The caregiver contact requirement specific to day treatment is focused on the contact being related to the beneficiary’s progress in day treatment and to support the role of the caregiver in supporting the beneficiary’s treatment goals. Documentation of the contact should be included in the day treatment documentation. Collateral contacts that are not part of day treatment must be documented in accordance with the documentation requirements of the specific specialty mental health service being provided to the beneficiary. If the collateral contacts are delivered as mental health services that require prior authorization, prior authorization must be obtained. If day treatment staff also delivers collateral or direct services that are not part of the day treatment program, the provider must establish fiscal tracking mechanisms that maintain a clear distinction between staff time and related resources attributable to the day treatment program and staff time and related resources attributable to other services. For example, the staff may be required to report the actual minutes/hours in each day spent on each type of service.
Under what conditions can classroom time be counted towards day treatment time?
A. Academic educational activities cannot be counted towards day treatment time.
Doesn’t the authorization by the ACBHCS process usurp the role of the IEP which, by federal and state statute, determines the services a special education eligible child will receive?
A. No, the authorization by the MHP described in the MHP Contract relates only to Medi-Cal payment for Medi-Cal eligible children. The Individualized Education Plan (IEP) Team process is independent of the Medi-Cal authorization process. As long as the IEP identifies the need for a mental health service and county mental health is the appropriate resource and concurs with the identified need, then county mental health is responsible for ensuring the provision of the identified service.
What would be an example of a typical day of three continuous hours of group work for young kids with impulse control problems, rapid mood fluctuations, hyperactivity, and frequent need for individual attention or redirection?
A. The therapeutic milieu components can be provided while the children are engaged in various activities, as long as the components are made available for the required time period during the course of the day treatment.
Can providers charge a fee to Medi-Cal beneficiaries for meals served at day rehabilitation or day treatment intensive program sites during the hours that the program operates?
A. Providers may not bill Medi-Cal beneficiaries or their conservators or otherwise require Medi-Cal beneficiaries to pay a fee for meals served during day rehabilitation or day treatment intensive program hours of operation.
Client Plans
When a young child is in Foster Care, and has a Child Welfare Worker as well as Foster parents and Biological parents is there some kind of "Practice Guideline" regarding who signs the Client Plan?
A. Since the Client Plan is not a legal document and belongs to the client, the client signs the Plan. (This is different from informed consent.) Even a young child can show understanding and ownership of the Plan. The child client can sign with their name, a scribble, etc. if they understand that signing it shows that the Plan belongs to them. A statement written by the clinician documenting why it is clinically inappropriate to obtain client’s signature is sufficient, especially for preverbal children. However, if treatment includes child-parent work then it could be appropriate to obtain the signature of the parent involved in treatment. Additionally, if a clinician finds it clinically appropriate to review the Plan with foster parents or bio parents, then their signatures can be obtained, but are not required.
Timeliness FAQs 
CSI Assessment Record Data FAQ
General Questions CSI Assessment Record Data FAQ
General Questions
When do we collect timeliness data?
A.Timeliness data should be collected for all new and returning new Medi-Cal clients (see list of definitions) that are requesting outpatient mental health services.
When a client enters the system through one program and then gets referred out (either directly to another program or through ACCESS) how does data get collected across programs?
A. The initial demographic data, type of service, and date of first contact to request services will be collected by the original agency and the remaining data points will be collected by the agency receiving the referral. Every provider needs a process for passing on the information to the agency which the client was referred for services (i.e.: fax, letter, encrypted email, etc.).
Do we need to request a PSP number at the beginning for all new clients in order to input data into the e-form and INSYST?
A. Yes. Do the registration form in InSyst and/or create an internal tracking system until such time that you have enough information to complete the registration form.
Providers have walk-ins at their clinics. For those that do not have openings, they refer them to ACCESS and ACCESS then refers those clients to other providers. Is the date of request the date the client went to the walk-in clinic or the date that ACCESS passes the referral to the other provider?
A. In this case, the date of request is the date the client went to the walk-in clinic.
What happens if it is found that this part of our system is consistently out of compliance with this standard? What are the consequences and who will be held accountable?
A. It is possible that we will be held fiscally accountable by the state for up to $500 per incident of non-compliance. However, the intent of gathering this information is simply to identify the areas of our system that are not meeting these requirements and make adjustments to come into compliance.
For programs that offer both psychiatric medication services as well as other specialty mental health services, what is the Type of Service code used (1, 2 or 3)?
A. The Type of Service depends on the type of service that the client is requesting at the “Date of First Contact to Request Services.” Typically this will be psychiatry services and then the other mental health services are added on as needed after the assessment is completed or as the need arises.
If my program is structured in a way that the Offer Date, Assessment Date, and Treatment Date will be the same. Is that a problem?
A. This is not a problem if this is what is occurring. It is important that you are utilizing the definitions provided by ACBH for each of these data points. Also, make sure that a treatment plan is in place before providing any planned services (there are exceptions -see doc manual) and remember that the Treatment Start Date is most often the date that the first planned service is provided.
Do we need to collect timeliness data for a walk-in consumer? Some of the walk-ins have private insurance or Medi/Medi and we do not serve them. What should we do in this case?
A1. If it is determined that a consumer who has requested services from your agency will be served within the ACBH System of Care, then the timeliness data should be collected.
A2. If there is any possibility that the client will get Medi-Cal, you need to collect all the information needed to report timeliness data and pass on to accepting agency/provider who will render services. If the client leaves the walk-in clinic prior to reporting information and before client is given a referral it would be impossible to pass on the information, then you would not need to.
A3. For those situations where not enough information was gathered or the person is not eligible: there is a field on the CSI Timeliness eForm “type of request” (Req-Sevc_Referred/ Not Eligible/ No Contact) there is an option here where minimal information is required. This does not require a client number in order to complete the form.
Please define ‘Prior Authorization’ on Page 2 of the Policy Letter.
A. Prior Authorization refers to services that require an authorization prior to services being rendered. DHCS MHSUDS Information Notice 19-026 Authorization of Specialty Mental Health Services indicate the prior authorization requirement for the following outpatient services: Day Rehabilitation, Day Treatment Intensive Therapeutic Behavioral Services, Therapeutic Foster Care, and Intensive Home-Based Services.
Does the Assessment Appointment ACCEPTED DATE change if client accepts a date, then misses that appoint, then accepts another appointment?
A. No. The date would remain the same even if they do not show up for the accepted appointment.
For clients in Residential programs only, are they considered new clients?
A1. According to the CSI Data Dictionary, Residential is not listed under Outpatient Services (CSI Data Dictionary S-06.0 Service Function).
A2. They are considered new clients if they have not received outpatient services in 12 months or are new to the MHP.
For clients that do not have Medi-Cal initially, but later end up obtaining Medi-Cal, do providers have to do the timeliness form once they have Medi-Cal?
A. Fill out the form as soon as someone is requesting mental health services if they are a new or returning new client, regardless of their Medi-Cal status.
For clients that do not have Medi-Cal initially, but then obtain Medi-Cal later, what would be the date of request for those clients?
A. The date of request for services would be the date of first contact, regardless of their Medi-Cal status.
Providers are asked to select psychiatry, outpatient services, or outpatient services-prior authorization, but what about FSP or other providers where they are a bundled service (psychiatry and other specialty mental health services), what do they select since the timeline is different for psychiatry and outpatient?
A1. Typically, clients don’t request FSPs for themselves. Usually a client needs all the services offered (psychiatry, case management and MH services).
A2. choose “outpatient services” for this one.
Are there confidentiality concerns in reporting this information to the State for Non-Medi-Cal, private pay clients?
A. Under HIPAA, a covered entity is permitted to use and disclose protected health information, without an individual’s authorization, for the purposes of “health care operations” which includes quality assessment and improvement activities and “competency assurance activities” which includes provider or health plan performance evaluation.
How will this timeliness data be audited?
A. Alameda County Behavioral Health Care Services is monitoring CSI Assessment Record Data collection via reports for use by providers and ACBHCS staff.
Adult System of Care Questions
When does the clock start ticking for the 10/15 day window to offer the first appointment? When someone is P-Coded to us? Or when we are first able to contact them? Or when they are open to a Team (intake)?
A. When the beneficiary agrees to the service when they sign the consent/Informing Materials (which is almost always the day the T code is opened). ACCESS assigns the P code often times prior to the client agreeing to the service. The program does assertive outreach and engagement once the P code is assigned and then usually the client agrees to treatment and the T code is opened the day they sign consent.
What if the client is at a psychiatric inpatient setting or in jail at the time of referral? Does engagement at a lockout setting count as a first appointment?
A1. Date of request of services would be the date that the first stepdown service is requested
A1. Assessment start and end date and treatment start date could all happen on one day.
Do services through AFBH (Adult Forensic Behavioral Health), BHC (Behavioral Health Court) or CAP (Court Advocacy Project) count as receiving services in the past twelve months?
A. No because they are not using their Medi-Cal insurance for these programs.
How do lockouts apply? If services are started in jail, for example, how does this affect these dates?
A1. First, determine if the client is a new client/new returning client.
A2. When a beneficiary enters the system via a crisis stabilization or in-patient service, this is not the Date of First Contact to Request Services. The Date of First Contact to Request Services is initiated on the date that the first stepdown service is requested; i.e., the beneficiary is discharged and a follow-up appointment/stepdown service is requested by the provider, client, or other referral source - that date is considered the Date of First Contact to Request Services.
For clients that received services from IHOT or other engagement only programs, are they considered new clients?
A. Yes. IHOT does not provide treatment services, but rather outreach and engagement services.
If a new client came through Mobile Crisis and then referred out, are they still considered a new client?
A. Yes. When the “new” beneficiary interacts with Mobile Crisis and willingly agrees to participate this would be date of request of services. If they agree to an assessment by mobile crisis that would be the assessment start date. If they receive crisis therapy by mobile crisis that would be treatment start date. If they are then referred to another agency Mobile crisis would forward those dates to ensure an assessment end date is completed.
What if the client is homeless and cannot be located right away?
A. If a program gets referred a client they cannot locate than that client would only be opened to their P code. Then when the client is located and able to engage and agrees to services and signs consent the T code would be opened and the day the client signs consent would be the day the clock would start.
Children System of Care
School based programs receive their referrals through the school district. Often during an IEP meeting with the client legal guardian, the school district discusses resources and mental health services and legal guardian agreement is obtained then. Is that date considered the date of request?
A. In this situation, if there is a therapist/clinician present from a contracted mental health agency, the date of the IEP meeting is the date of request (assuming the legal guardian agreed). If there are only school district employees present for the IEP meeting, the date of request would not be until the legal guardian expresses agreement to have their child receive mental health services to the person from the contracted mental health agency once they reach out to the family to engage them in services. In other words, the date of request is the date that the system becomes aware that the legal guardian of the child wants mental health services to be provided.
How does presumptive transfer fit in with Timeliness reporting?
A1. Presumptive transfer (PT) - If a child/youth beneficiary is presumptively transferred to an MHP, that MHP is responsible for providing, or arranging for, SMHS.
A2. If a child has not received outpatient mental health services in Alameda County and there is a presumptive transfer from another county. When that child is referred to the program and a legal guardian/or parent agrees to services that is the date of requested services.
A3. These beneficiaries should be included in geo-mapping based on placement. If Presumptive Transfer is waived and the MHP contracts with providers out-of-county (not within time & distance standards), these providers should NOT be included in the NACT.
For ERMHS clients who are referred to a provider for services from county’s Children Specialized Services (CSS) unit, are they considered new if they were assessed by CSS to determine ERMHS eligibility?
A1. When a child is new/new returning and the legal guardian or parent agrees to ERMHS assessment, that would be the date of requested services. The ERMHS assessor should keep track of the date of request and pass that along to the next agency. It may be some time since the school district is in control of who and when gets referred out to the agencies. It is requested that the agency reaches out to ERMHS assessment team to get the date of request information.
A2. The person completing the ERMHS assessment can inform the caregiver of the length of time it takes to get through the school district system, and offer the caregiver services outside of the school through ACCESS. The date of request services would then be passed on to ACCESS.
ACCESS/Language Specific ACCESS Program Questions
If a referral came through ACCESS, how do we know if it’s urgent? Will ACCESS indicate “urgent” on their referral form?
A. Yes, ACCESS will indicate if a request is “urgent” on the Referral Letter sent to the provider.
Could the Contact Tracking Database be aligned with the timeliness requirements for ACCESS programs?
A. We will take this under advisement and, if it is a possibility, it will not happen for some time.
If a referral came through ACCESS, will ACCESS indicate the type of service requested on their referral form?
A. It can usually be determined what type of service ACCESS is requesting based on who the referral is sent to (e.g. if a person needs a forensic FSP we would send to one of the forensic FSP programs). In situations where there may not be clarity, such as if ACCESS refers a consumer to an individual provider who does therapy and psych testing, the type of service being requested for that consumer is always indicated on the referral letter.
Providers receive referrals through ACCESS, Help Me Grow, etc. and sometimes there is a lag from ACCESS to providers, which greatly impacts the timeliness requirement. What is the ACCESS referral process and what is the timeline from request from client/legal guardian to ACCESS and to providers?
A. ACCESS sends out Referral letters (by fax or email) the same day or within 2 days of the request; if there are insurance issues or more information is needed to determine level of care, it may take longer (those are the exceptions).
What is the Referral Source code for ACCESS?
A. The referral source code for ACCESS is 14 = Other County / Community Agency
COVID-19 FAQs

ACBH FAQs: Clinical Documentation Updates
During the COVID-19 Nationwide Public Health Emergency
Principles:ACBH recognizes that COVID-19 presents a myriad of challenges. ACBH is working collaboratively with Department of Healthcare Services (DHCS), providers, and other stakeholders to ensure we continue to protect access to care and services, while also minimizing COVID-19 spread.
May providers claim for telephone and telehealth services?
Yes, both SMHS and SUD services may be provided via telehealth. Please refer to the following ACBH and DHCS resources:
- Leveraging Technology to Meet Client Needs – New Guidance from DHHS-OCR (issued on March 18, 2020)
- Leveraging Technology to Meet Client Needs – Non-Licensed Staff Update (issued on March 19, 2020)
May providers claim for services provided via text messaging to clients during the COVID-19 emergency?
No. We have now received updated guidance from DHCS that there is no claiming for texting clients at this time. Texting is only allowed for scheduling appointments with clients. DHCS Legal is vetting any additional use of texting.
May providers claim for services provided via email messaging to clients during the COVID-19 emergency?
No. At this time, DHCS has not given permission for claiming for email communication. When a beneficiary consents to the use of email communication, and that consent has been documented, counties may send SMHS and SUD notices via email. Providers must remain HIPAA and 42 CFR Part 2 compliant.
May a LPHA provider whose license has expired continue to provide services if they are unable to renew their credential with their licensing board at this time?
Yes. for additional information, please see below:
1. Order Waiving License Renewal Requirements 2. Order Waiving License Reactivation or Restoration Requirements
Will late signatures (Informing Materials Consents, Client Plan and Medication Consents) be accepted as compliant for claiming purposes if verbal consent is provided?
Yes, for those documents listed above—but not for Release of Information forms (ROI). In the session’s progress note, explain specifically what information was shared with the client, that the client verbally consented to the information provided, and that due to the COVID-19 emergency the client was unable to meet in-person and sign the document. As well, during this public health crisis ACBH has temporarily suspended the requirement for client signature for receipt of psychiatric medication during this time of emergency (Cal. Code. Regs. tit. 9 § 852).
May the platform DocuSign be utilized to obtain electronic signatures?
Yes, during the COVID emergency, HIPAA-compliant electronic signature platforms such as DocuSign may be used for both staff and client electronic signatures. However, a Business Associate Agreement must be in place with the electronic signature vendor in order to utilize HIPAA-compliant platforms.
When the emergency ends, does ACBH expect that providers will go back and obtain treatment or client plan signatures for clients that are still in treatment?
No, Providers are not expected to get signatures from beneficiaries who receive Specialty Mental Health Services and SUD services during the time period of the COVID-19 public health emergency. When the public emergency ends, providers shall resume compliance with all documentation and signature requirements and update all clinical records on a “go-forward” basis.
Can the client provide verbal consent for a Release of Information (ROI)?
No. The U.S. Department of Health and Human Services has not waived the signature requirements of written authorizations for client releases of information. You may discuss the release of information with the client and mail the forms to them for their signature (it is suggested you enclose a self-addressed stamped return envelope as well). A copy, fax, or photo sent by email or text will be acceptable for a signed ROI. A witness signature is not required on the ROI form.
(MH only) Under what circumstances could a provider disclose PHI to a family member, relative, close friend, or other person identified by the individual without an ROI?
A provider may disclose PHI to a family member, relative, close friend, or other person identified by the MH (not SUD) client as responsible for their care without an ROI under the following circumstances when the client is NOT present:
1. The family member, relative, close friend, or other person has already been identified by the client as responsible for their care;
2. The PHI is used to notify or assist in the notification of (i.e. identifying/locating) this family member/person responsible for the client's care of the client's location, general condition or death;
3. The provider determines in their professional judgment that the disclosure is in the best interest of the client; AND
4. The provider discloses ONLY the PHI directly relevant to the person's involvement with the client's care or payment related to the client's care or for notification (i.e. minimum necessary).
5. For example, the provider may infer that it is in the client's best interest to allow the other person to act on behalf of the client in picking up filled prescriptions, medical supplies, or other similar forms of PHI
6. See 45 CFR 164.510(b)(3)). https://www.law.cornell.edu/cfr/text/45/164.510
Yes, but only if they do not disclose any PHI to the person with whom they are speaking. This includes NOT disclosing that the caller works for a behavioral health services provider.
Has ACBH issued any additional guidance on Telehealth and HIPAA privacy and security?
Yes, the Alameda County Health Services Agency Office of Compliance Services issued the following guidance: Remote Work and HIPAA Privacy and Security: March 2020 FAQs: COVID-19 Telehealth and HIPAA Privacy & Security
Are there any exceptions to obtaining client written consent before disclosing Protected Health Information (PHI)?
1. Specialty Mental Health Services (SMHS): Yes, a MH provider may disclose PHI to another HIPAA-covered health care professional (mental and/or physical health) for the purpose of treatment, and for health care operations activities including care coordination (e.g. referrals) for mutual clients
2. Substance Use Disorder Services (SUD): Yes, a SUD provider may disclose PHI without written consent to medical personnel in order to treat a bona fide medical emergency based on the SUD provider’s discretion. However, this provision may NOT be used to override a client’s objection to disclosure. 3. (See SAMHSA Guidance: COVID 19 Public Health Emergency Response and 42 CFR Part 2 Guidance.)
During the COVID-19 emergency many of our clients desperately need case management services to link them with critical community services. If I am unable to meet with the client in person to obtain a written ROI, how can I advocate on their behalf for services that do not meet the above exceptions?
If you are speaking with the client on the telephone or via telehealth, you may ask their consent to add another service provider to a multiparty conference call. An ROI is not required in this situation because the client is on the original phone call, implying consent.
When providing Telehealth services, do I use the face-to-face or non-face-to-face codes?
Telehealth services, including for assessments such as CANS and ANSA, will be coded as face-to-face service. Please note, that location code 20 is indicated in the medical record when claiming for telehealth services.
Are written Telehealth Consents required before Telehealth Services begin?
No, during the emergency period, the requirement for written or verbal consent is suspended for Telehealth Services. The requirement for written consents for Telehealth Services will resume after the emergency ends. (See Executive Order N-43-20.)
Is there an ACBH required Telehealth Consent form to use?
No. ACBH is in the process of developing a Telehealth Consent Form for future use.
During the COVID-19 emergency has there been any changes to the NOABD and State Fair Hearing Appeal process?
Yes, from March 1, 2020 through the conclusion of the COVID-19 emergency clients will have 240 days (rather than 120 days) to file for a State Fair Hearing when their Appeal is denied by ACBH. When NOABD’s are issued to the client—an additional insert must be added. See: ACBH Grievance System
Where can I find COVID testing resources?
1. http://www.acphd.org/2019-ncov/testing.aspx
2. http://www.acphd.org/media/571443/alameda-county-covid-testing.pdf
(SUD only) Can ACBH clarify that assessment and medical necessity and level of care may also be done by telephone for Drug Medi-Cal Organized Delivery System (DMC-ODS) providers
Yes. In anticipation of CMS’ approval of DHCS’s 1135 Waiver request, beginning on March 1, 2020 and for the duration of the emergency, the initial assessment of the beneficiary may be performed by telephone by an LPHA with the appropriate scope of practice.
(SUD only) Can the consultation between an LPHA and counselor that is needed for level of care determinations also be done by Telehealth)?
Yes, the LPHA can review the assessment with the counselor through a face-to-face telehealth discussion when establishing the SUD diagnosis, medical necessity, and level of care assignment.
(SUD only) Can individual counseling services be provided via telehealth and telephone?
Yes. Individual Counseling may be provided via telehealth by ACBH SUD providers.
Can group counseling services be conducted via telehealth and telephone? If so, does the 12-client limit remain in place?
Yes. Group Counseling services may be provided for SUD and Specialty Mental Health Services and the 12-client group size limit still applies for SUD.
How can providers ensure their patients do not run out of medications?
1. Medi-Cal allows patients to fill up to 100 days of non-controlled medications. Narcotic treatment programs can receive exemptions to provide take-home medications for patients who are sick or quarantined. See DHCS COVID-19 FAQ: Narcotic Treatment Programs for more detail. Patients receiving buprenorphine products can currently receive 30-day supplies on Medi-Cal.
2. Utilization limits on quantity, frequency, and duration of medications may be waived by means of an approved Treatment Authorization Request (TAR) if there is a documented medical necessity to do so. See DHCS pharmacy guidance.
Can controlled substances be prescribed over the phone?
This is a federal, not state, issue. SAMHSA released guidance that an initial evaluation by telehealth or telephone is allowed for buprenorphine during the emergency. The DEA COVID-19 website addresses all other controlled substances, which include sedatives and stimulants, under telemedicine. Practitioners can start a new controlled medication prescription by telephone for a patient who is already under their care by telephone. However, if a patient is new to the provider, controlled medications cannot be provided by telephone (other than buprenorphine). For patients new to the provider, prescribing controlled medications can only be done by live video or telemedicine.
Does ACBH have specific expectations for documentation of services delivered by telephone or telehealth?
Providers may indicate that telephone and telehealth services were provided in lieu of in-person services due to COVID-19 social distancing practices and continue following current documentation requirements.
(SUD only) Can DHCS waive the requirement that SUD treatment programs maintain a minimum of 30% licensed staff?
No, pursuant to California Code of Regulations Title 9, Chapter 8, Section 13010, at least 30% of staff providing counseling services in all AOD programs shall be licensed or certified.
Are facilities able to provide treatment or recovery services outside the facility service location if there are concerns about providing treatment at the location due to COVID-19?
In some circumstances, DHCS shall consider and may allow facilities to provide treatment or recovery services off-site for any concerns related to COVID-19. Providers should contact their Licensing Analyst for questions. See COVID-19 Response website for information notices for treatment facilities.
(MH only) Can a licensed mental health professional provide direction to a Therapeutic Foster Care (TFC) parent through telehealth rather than in person?
Yes. Telehealth and telephone may be used by licensed mental health professionals to provide direction to TFC parents during the emergency.
(SUD only) During the emergency, are DMC-ODS providers still required to discharge beneficiaries if there is a lapse in treatment for more than 30 days?
Yes. DMC-ODS providers are required to discharge beneficiaries when there is a lapse in treatment for more than 30 days, although beneficiaries can be readmitted. Beneficiaries should be reassessed for readmission when ready to resume treatment. Note: the two non-continuous residential stay limit still applies in DMC-ODS (1115 Waiver, Standard Terms and Condition (STC) 138-Residential Treatment).
(MH only) Is DHCS waiving the 23-hour maximum length of stay in a Crisis Stabilization Unit (CSU) during the emergency?
No. DHCS is not waiving the maximum length of stay requirement in a CSU, specified in California Code of Regulations, Title 9, Section 1810.210. However, in cases where a beneficiary remains in a CSU for more than 23 hours, the provider must be able to present evidence upon request by DHCS of good faith efforts they have made to transition the beneficiary out of the CSU to their residence or to an appropriate placement, including the reason(s) why that has not been possible.
(MH only) Are psychiatric health facilities (PHF) and CSUs allowed to offer services outside of the licensed part of the facility at locations that are already Medi-Cal certified for outpatient services?
DHCS will review requests regarding PHF licensing on a case-by-case basis (LCDQuestions@dhcs.ca.gov). For Medi-Cal Certification related questions, including those pertaining to CSUs, DHCS will review requests on a case-by-case basis (DMHCertification@dhcs.ca.gov).
(MH only) DHCS requests proof that there is a psychiatrist and licensed person (LCSW, LMFT) on the PHF unit each day, which is later audited for the hours of attendance. May psychiatrists be available by telehealth, off-site? And can this obligation be addressed by having two licensed staff at a time?
DHCS will review requests regarding PHF licensing requirements on a case-by-case basis (LCDQuestions@dhcs.ca.gov).
(SUD only) During the emergency, is it possible for DMC-ODS to use non-registered or non-certified staff with lived experience working under the supervision of licensed and/or certified staff to provide services in Recovery Support and Case Management?
The current requirements for providing Recovery Support and Case Management services have not changed during the public health emergency.
(SUD only) During the emergency, may Alcohol or Other Drug (AOD) counselors to provide services after their certification expires, while waiting for the renewal?
As outlined in MHSUDS IN 18-056, if an AOD counselor fails to submit a renewal application prior to the expiration of their certification, the counselor may not provide counseling services until their certification is renewed. But, if an AOD counselor submits a renewal application prior to the expiration of their license, the counselor may continue to provide counseling services unless the certifying organization denies the renewal application. If the counselor’s certification is denied, any service provided after the expiration date of the counselor’s certification shall not be reimbursed with State or federal funds.
How do providers access federal grant opportunities?
1. Providers should stay updated by regularly checking the federal websites for grant opportunities. DHCS has a web page that reflects a compilation of websites that may be followed to search for grant funding opportunities. These links can provide more information on the following opportunities: provider relief fund; Grants.gov; telehealth; small business loans; and SAMHSA grant announcements.
2. The Small Business Administration recently issued two interim final rules to supplement previously posted interim final rules on the Paycheck Protection Program (PPP) with additional guidance regarding disbursements, as well as guidance on the amount of PPP loans that any single corporate group may receive and criteria for non-bank lender participation in the PPP.
Where are up-to-date resources on COVID-19?
1. California Department of Public Health – COVID-19 Updates CDPH
2. Gathering/Meeting Guidance
3. CDC COVID-19 webpage
4. Guidance for the Elderly
5. Guidance for Employers
6. What to do if you are sick
7. Guidance for Workplace/School/Home Document
8. Steps to Prevent Illness
9. Guidance for use of Certain Industrial Respirators by Health Care Personnel Medicaid.gov, COVID-19 resource page
10. CMS: Emergency Medical Treatment and Labor Act (EMTALA) Requirements and Implications
11. Governor Newsom’s 3/12/20 Order
12. CDPH: For Individuals with Access and Functional Needs
Does DHCS provide an outreach letter to Medi-Cal Beneficiaries regarding COVID-19?
Yes, see https://www.dhcs.ca.gov/Documents/Beneficiary-Outreach-Letter.pdf
This is an excellent resource to provide to clients during the COVID emergency.
Are there COVID resources for Spanish speaking individuals?
Yes. MUA Publishes a COVID19 Resource Guide for the Immigrant Community https://bit.ly/MUAGuiaCOVID19
Are there support resources for staff and providers during the COVID emergency?
Yes. See local staff COVID support resources below.
1. In collaboration with Alameda County Psychological Association (ACPA), Crisis Support Services of Alameda County (CSS) is rolling out the Staying Strong Against COVID19 Support Line for Bay Area Workers in Healthcare Settings.
It's Okay to Vent: 510-420-3222
2. The COVID19 Pro Bono Counseling Project is an organization offering free video and phone therapy to front-line healthcare workers in the Bay Area during the COVID19 crisis. See: https://sites.google.com/view/cpbc-proj/home and https://www.youtube.com/watch?v=5rgI5T1Vxgo&feature=youtu.be
How should behavioral health programs reduce transmission of COVID-19?
The CDC has provided interim infection prevention and control recommendations in health care settings. As well, all providers are now required to wear facial coverings inside their programs and sites.
How should behavioral health providers manage clients presenting with upper respiratory symptoms?
ACBH strongly encourages use of telehealth or telephone services to minimize infection spread. Programs should follow infection prevention and control recommendations in health care settings published by the CDC (please see Q35 for more details).
When should programs refer a patient to medical care?
See CDC guidelines for health care professionals on when patients with suspected COVID-19 should seek medical care.
What should facilities do in the event a client is diagnosed with COVID-19?
If a client of an outpatient facility is confirmed to be positive for COVID-19, the client should be instructed to stay home. As much as is possible services should be provided by telephone or telehealth. Residential or inpatient facilities with a patient or resident diagnosed with COVID-19 should ensure the patient is isolated in a room, has a mask for use when leaving the room, and should contact their local public health department for guidance. It is the duty of every health care provider, knowing of or in attendance on a case or suspected case of any of the diseases to report to the local health officer (17 CCR § 2500 (b)). For COVID-19, immediate reporting by phone (17 CCR § 2500 (b)). Inpatient and residential facilities must also report to DHCS, within one (1) working day, any events identified in California Code of Regulations Title 9 Chapter 5 Section 10561(b)(1), which would include cases of communicable diseases such as COVID-19.
If a former client is later found to have been diagnosed with COVID-19, what action should be taken?
1. Staff should inform individuals of possible exposure but must do so in a way that protects and maintains the other clients’ confidentiality as required by law. Clients exposed to a person with confirmed COVID-19 should refer to CDC guidance on how to address their potential exposure, as recommendations are evolving over time.
2. It is the duty of every health care provider, knowing of or in attendance on a case or suspected case of any of the diseases to report to the local health officer (17 CCR § 2500 (b)). For COVID-19, immediate reporting by phone (17 CCR § 2500 (b)).
3. Inpatient and residential facilities must also report to DHCS, within one (1) working day, any events identified in California Code of Regulations Title 9 Chapter 5 Section 10561(b)(1), which would include cases of communicable diseases such as COVID- 19.
What should facilities do in the event a staff member is diagnosed with COVID-19?
Staff members who have symptoms of a respiratory illness should stay home until symptoms completely resolve. Staff members with confirmed COVID-19 infection, or who are under investigation (testing pending), should stay home and the facility should contact their local public health department for guidance.
It is the duty of every health care provider, knowing of or in attendance on a case or suspected case of any of the diseases to report to the local health officer (17 CCR § 2500 (b)). For COVID-19, immediate reporting by phone (17 CCR § 2500 (b)).
Inpatient and residential facilities must also report to DHCS, within one (1) working day, any events identified in California Code of Regulations Title 9 Chapter 5 Section 10561(b)(1), which would include cases of communicable diseases such as COVID- 19.
What else can behavioral health programs do to prepare for or respond to COVID-19?
DHCS encourages providers to adhere to the CDC’s and CDPH’s recommendations to prepare for COVID-19.
How can behavioral health providers obtain personal protective equipment (PPE)?
Resources on infection mitigation in behavioral health facilities are as follows:
1. California Department of Public Health (CDPH) Health Care System Mitigation Playbook which provides helpful information to medical facilities on infection control and mitigation, and has useful information for BH facilities as well.
2. ASAM’s, Infection Mitigation in Residential Treatment Facilities which provides helpful information on the same, designed for SUD residential treatment.
3. National Council on Behavioral Health COVID-19 guidance for behavioral health facilities.